Are we finally getting closer to finding a cure for the debilitating disease that Stephen Hawking suffered from?
UL MF researchers involved in the discovery of new genes associated with amyotrophic lateral sclerosis (ALS).
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disease that affects one in 350 people. The causes of ALS are largely unknown, which makes it impossible to develop effective treatments. ALS develops when motor neurons (i.e., specific nerve cells in the brain and spinal cord) begin to deteriorate. Typical symptoms include muscle weakness, atrophy, and later muscle paralysis, which eventually leads to death from respiratory failure. The course of the disease is difficult to predict. The world-famous physicist Stephen Hawking was already diagnosed when he was 21, and doctors predicted he only had a couple of years to live. Despite the disease, he lived to be 76. However, most patients only live two to five years after being diagnosed.
In cooperation with the Ljubljana University Medical Centre Institute of Clinical Neurophysiology, researchers at the University of Ljubljana Faculty of Medicine have already been studying the genetic and epigenetic causes of ALS since 2010, and research on ALS at the cellular level is also being conducted at the Jožef Stefan Institute.
In 2013, ALS patients launched a worldwide crowdfunding campaign (Project MinE) to help researchers find the genetic causes of ALS. Researchers soon realised that the complexity of the disease required international collaboration and pooling of patients and matched controls from multiple countries. Collaboration between researchers from 22 countries (including Slovenia) resulted in the 2016 discovery of the C21orf2 gene, which increases the risk of developing this disease. The researchers' findings were presented in the article published in the journal Nature Genetics.
Collaboration continued, and in December 2021 a team of international researchers, which also included Slovenians and was led by Jan Veldink and Leonard van den Berg at the Utrecht Medical Centre, published new findings from a cross-ancestry genome-wide association study including a large sample of 29,612 ALS patients and 122,656 controls. Fifteen new genes were discovered, whose pathological variants increase the risk of ALS. An important new discovery is that unlike some other neurodegenerative diseases (e.g., Alzheimer's or Parkinson's disease), genetic factors in ALS are largely expressed in one type of cells in the central nervous system – that is, the glutamatergic neurons, which use glutamate to communicate with other cells. New genetic variants (see figure below) indicate impaired autophagy and perturbations in vesicle-mediated transport.
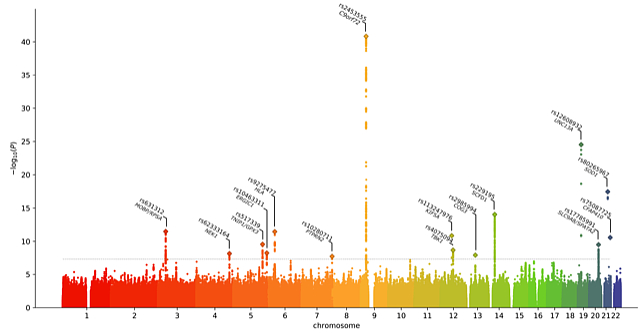
Figure: Results of the whole genome analysis (GWAS) in 29,612 ALS patients and 122,656 controls. Displayed are the SNPs* for 22 chromosomes and 15 pathological genetic variants that have statistically significant correlations with the development of ALS. *SNP = single-nucleotide polymorphism. Published with the permission of the author Wouter van Rheenen.
The study also revealed a causal relationship between high cholesterol levels and ALS. The causal relationship between the incidence of ALS and total cholesterol was determined using various statistical models. In total, 83 and 178 SNPs were used as instruments at cut-offs of P < 5 × 10−8 and P < 5 × 10−5, respectively. All methods showed a positive effect for an increased risk of ALS with higher total cholesterol levels. The role of cholesterol can be associated with impaired autophagy – that is, a process that cleans out cells or removes unnecessary or dysfunctional cellular components.
The biological processes of neuron-specific pathology revealed in the study can serve as potential targets for therapeutic strategies.
The Slovenian co-authors of the study published in the December issue of Nature Genetics include Metka Ravnik-Glavač and Damjan Glavač from the University of Ljubljana's Faculty of Medicine, Blaž Koritnik and Janez Zidar from the Ljubljana University Medical Centre Institute of Clinical Neurophysiology, and Boris Rogelj from the Jožef Štefan Institute and the University of Ljubljana's Faculty of Chemistry and Chemical Technology.